Sight Lost Slowly: How Glaucoma Turns Late Care into Lifelong Disability
By Arunima Rajan
Glaucoma’s tragedy lies in its timing: early disease is silent, while late disease is irreversible. The critical gaps are in screening, referrals, and long-term adherence to care.
Glaucoma causes damage quietly and progressively. For years, it can destroy vision without producing any obvious warning signs. Many patients seek medical help only when it is too late: when they can no longer climb stairs, read, or safely navigate traffic.
“Glaucoma is a group of eye diseases that damage the optic nerve, the structure that transmits visual information from the eye to the brain. In most cases, this damage is related to elevated or poorly tolerated eye pressure, though pressure alone does not tell the whole story. What makes glaucoma particularly dangerous is that vision loss typically begins in the peripheral vision and progresses slowly toward the center, without pain or noticeable symptoms. By the time patients become aware of a problem, substantial and irreversible optic nerve damage and vision loss have often already occurred,” says Andrew Smith, MD, ophthalmologist, UCI Health Gavin Herbert Eye Institute.
Glaucoma should be viewed as a spectrum of conditions rather than a single diagnosis, with risk shaped by both measurable factors and individual susceptibility, he adds. “Patients with a family history of glaucoma, elevated eye pressure, thin corneas, certain ethnic backgrounds, or systemic vascular disease should be monitored earlier and more closely. Importantly, “normal” eye pressure does not eliminate risk, especially in patients with optic nerve changes. Earlier awareness and risk-based screening are critical, because waiting for symptoms means waiting too long,” says Smith.
Take the case of 84-year-old Edwin*, who lives in Nagercoil, a small town in Tamil Nadu, with his 80-year-old wife. “I don’t allow him to step outside the house because he might fall,” says his wife, Catherine*. “At his age, a single fall can make him bedridden. He used to work for an NGO and rarely went for eye check-ups. There were no visible symptoms, and by the time he was diagnosed, significant vision loss had already occurred.”
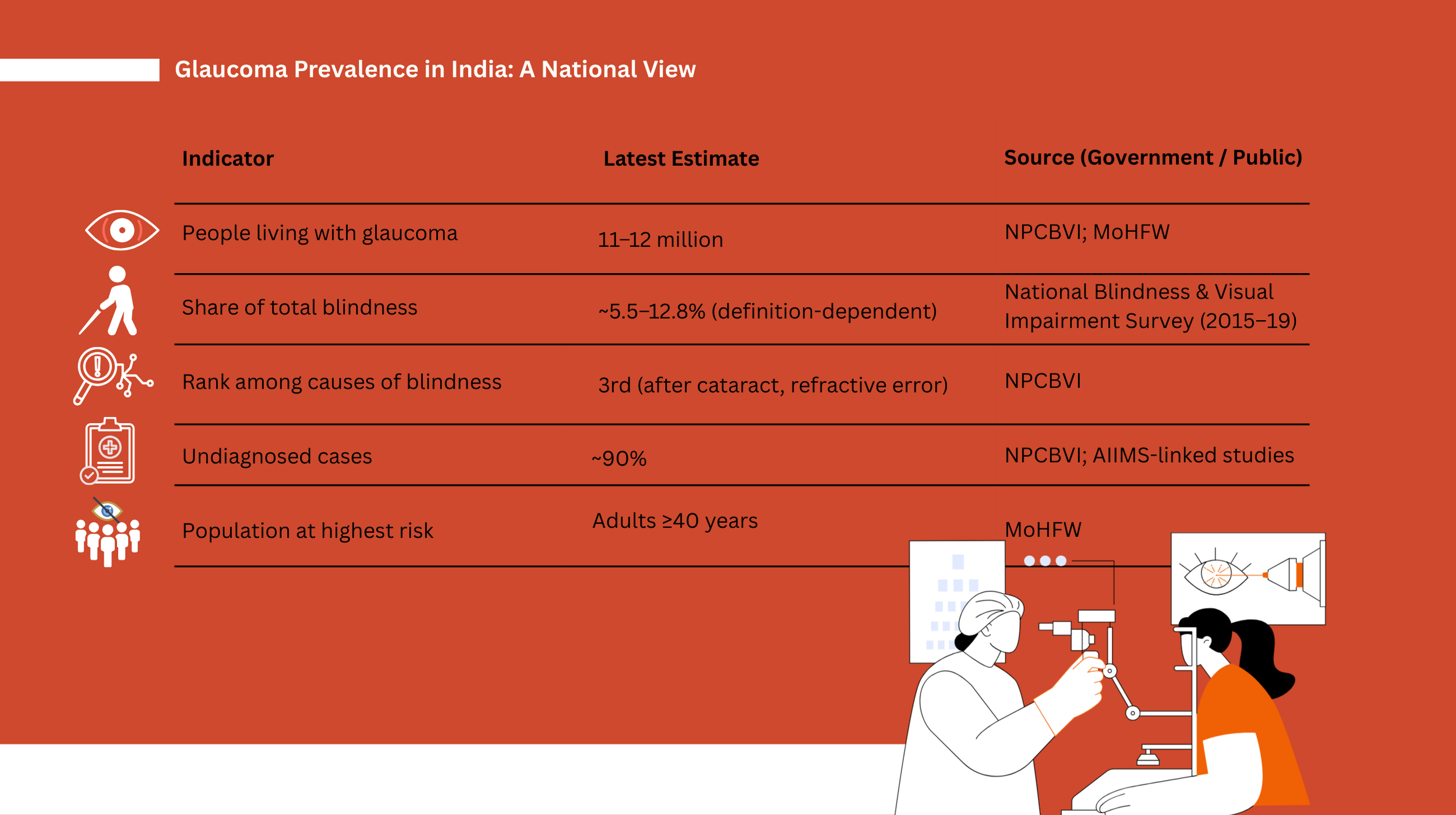
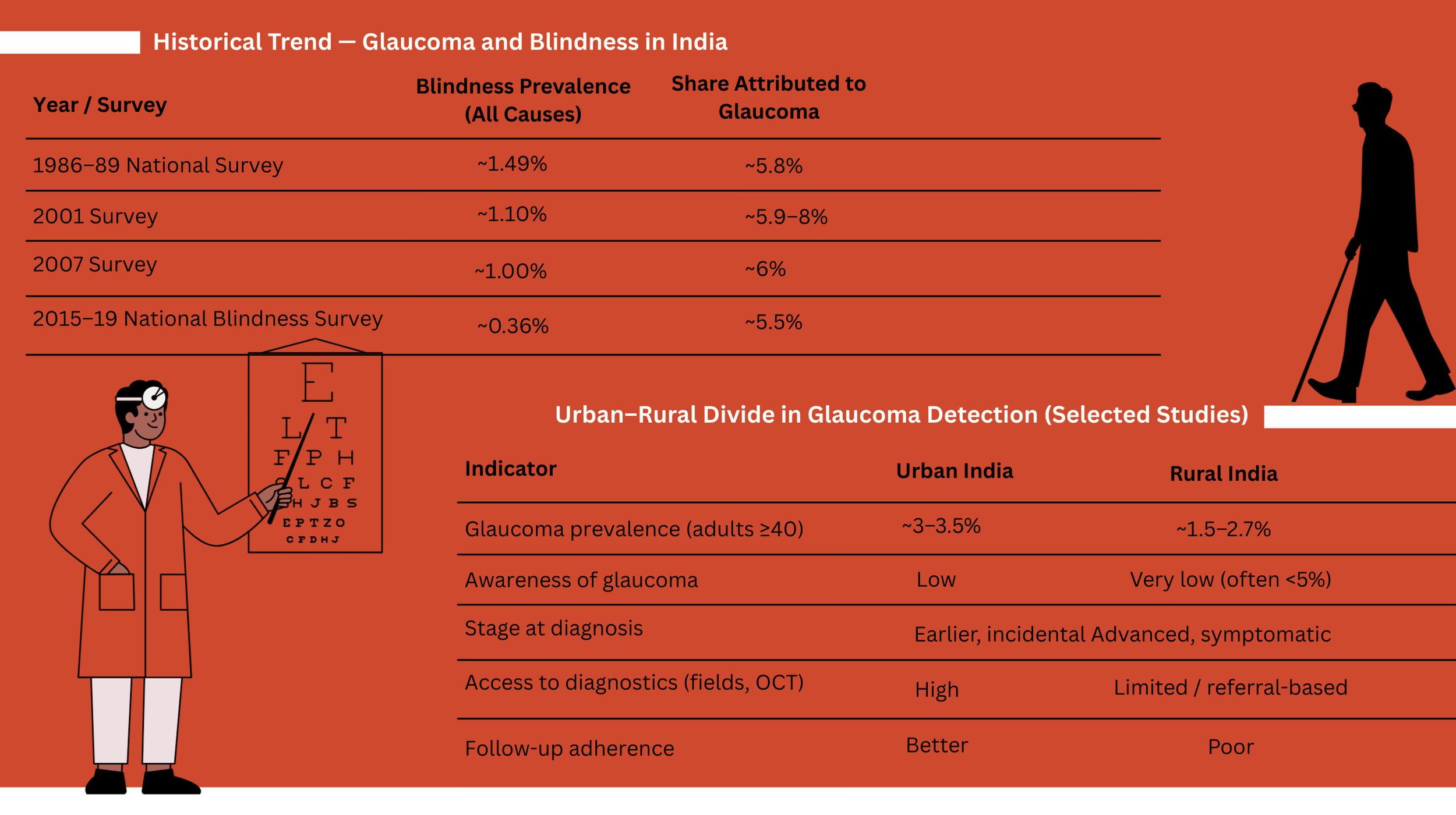
An estimated 11.2 to 12 million Indians over the age of 40 are affected by glaucoma. The disease accounts for approximately 12.8% of all blindness in India, yet nearly 90% of cases remain undiagnosed.
“Research from ASG Eye Hospital specialists indicates that nearly 70% to 80% of patients seek medical attention only after the disease has reached an advanced stage,” says Dr. Vikas Jain, COO, ASG Eye Hospital. “By the time patients notice ‘tunnel vision’ and consult a doctor, the optic nerve has often sustained permanent damage, with many having already lost up to 40% of their visual field. This late presentation is largely due to the brain’s ability to compensate for peripheral vision loss, allowing the disease to progress unnoticed until it reaches a critical and irreversible threshold.”
Gaps in the Glaucoma Care Pathway
“A patient who presents with end-stage glaucoma is a self-writing script. In other words, the optic nerves are severely damaged: nerve cupping is greater than 0.8, visual fields are less than 10 degrees, and intraocular pressures are either lifelong stage-4 highs or deceptively low-normal. Most of these patients are still driving, working, and going about their daily lives with no idea that anything is even slightly amiss. That represents years of damage, and not months. Peripheral vision does not disappear overnight. It erodes slowly, silently, and permanently,” says Gregg Feinerman, Medical Director of Feinerman Vision in Newport Beach, California.
Technology has improved, but overall it has not moved the needle enough. What has changed is our ability to detect damage earlier, if we are looking for it. Too often, we are not. Optical coherence tomography (OCT) imaging has been available for years and can detect nerve fiber loss at the micron level, but this only happens if a patient is referred into specialty care or happens to have red flags identified during a routine exam. Otherwise, glaucoma is still missed, he adds. “The average age at diagnosis has inched down by a few years, but not dramatically. Diagnosis today still looks much like it did 15 years ago: late, with advanced damage, often in both eyes,” says Feinerman.
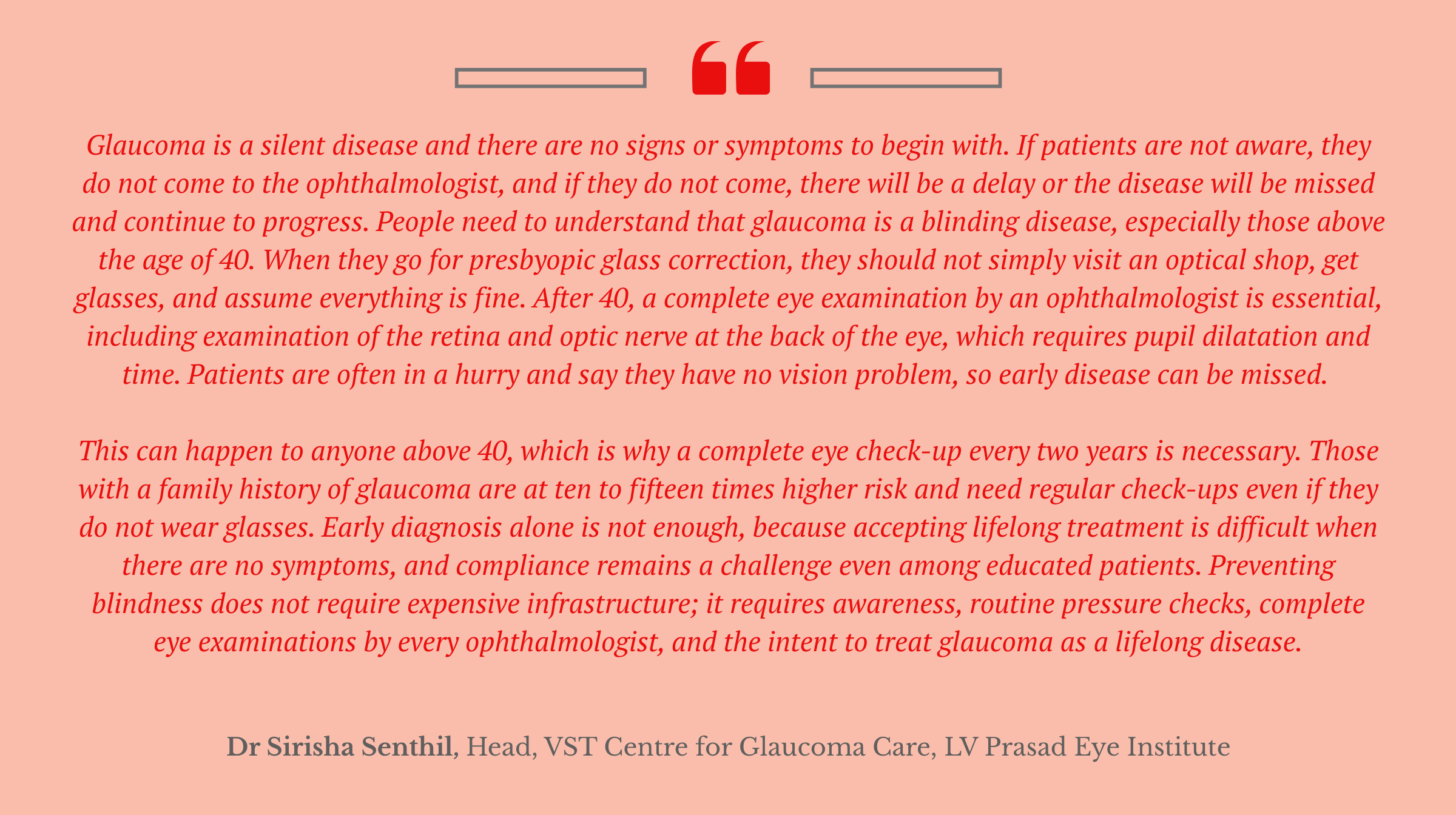
Early detection is essential to prevent irreversible vision loss. However, doctors point to multiple gaps in India’s glaucoma care pathway: ranging from awareness and routine screening to referral systems and long-term treatment adherence.
According to Dr. Jain, these gaps are both structural and behavioural. “There simply aren’t enough screenings, which is why nearly 90% of cases go undiagnosed. Mandatory, comprehensive optic nerve assessments during routine eye exams could significantly address this.”
Geographical disparities further compound the problem. Tier-2 and tier-3 cities often lack access to advanced diagnostic tools. Treatment adherence is another major challenge. “Eye drops are expensive, must be used every day for life, and don’t offer immediate improvement in vision. As a result, many patients discontinue treatment,” Jain explains. “This is worsened by the shortage of glaucoma specialists and the absence of robust digital systems to track disease progression over many years. Patients miss follow-ups, allowing this ‘silent thief’ to keep stealing their sight unnoticed.”
Two Kinds
“There are two main types of glaucoma, and depending on the type, early changes may be detected differently. Open-angle glaucoma (OAG) progresses very slowly and often causes few, if any, symptoms in its early stages. In fact, vision is often preserved until late in the disease, by which point the glaucoma is usually quite advanced and irreversible. Glaucoma-related vision loss typically begins in the peripheral vision before progressing toward central vision and, in severe cases, leading to legal blindness,” says Dr David Allamby, Medical Director at Focus Clinics, a leading laser eye clinic based in London.
He adds: A visual field test can accurately detect peripheral vision loss caused by glaucoma. During this test, dots of light are displayed around a bowl-shaped screen, and the patient clicks a switch each time a light is seen. Because OAG has few warning signs before damage occurs, it is vital to attend regular eye examinations. If glaucoma is detected early, an ophthalmologist can prescribe preventive treatment to help protect vision. The key point is that by the time a patient notices vision loss, the disease is already very advanced. Early detection is essential to preserve vision and prevent blindness.
“A special type of eye scan, known as optical coherence tomography (OCT), has revolutionised glaucoma detection and management. Many eyes show clear OCT progression before reproducible visual field loss, especially in early open-angle glaucoma. As a result, many opticians now have OCT scanners in their practices,” he says.
Closed-angle glaucoma, by contrast, can develop suddenly, and its symptoms are often very noticeable. These may include misty or blurred vision, rainbow-coloured circles around bright lights, nausea, severe eye and head pain, narrowing of vision, and sudden loss of sight, he adds.
“There are several treatments for glaucoma, including eye drops, laser treatment, and surgery. Treatment depends largely on the type of glaucoma diagnosed. Open-angle glaucoma is usually managed with eye drops or outpatient laser procedures, while closed-angle glaucoma often requires immediate hospital treatment, along with medication to rapidly reduce eye pressure. Most people with glaucoma will not go blind if they adhere to treatment and attend regular eye examinations,” says Dr Allamby.
The Family Connection
Dr. Pankaj Bendale, Glaucoma and Cataract Surgeon at the National Institute of Ophthalmology, Pune, echoes these concerns. “The biggest gap in India’s glaucoma care is early detection. Because the disease is asymptomatic in its initial stages, people often skip routine eye examinations, which is precisely when glaucoma can be identified and stabilised.”
He emphasises the importance of public education and family screening. “Regular check-ups should extend not only to patients but also to first-degree relatives and children. Timely diagnosis, followed by consistent treatment and frequent reassessment, is essential to prevent avoidable vision loss.”
Last-Mile Delivery Still a Challenge
Despite being a global leader in high-volume cataract surgery, India’s eye-care system is still evolving to meet the lifelong demands of chronic conditions such as glaucoma. While digital infrastructure can screen millions, last-mile delivery of continuous, affordable care remains a challenge.
This creates a paradox: India has the clinical and digital capability to screen widely, yet struggles to provide sustained care. Addressing this gap will require a shift away from episodic, visit-based treatment toward more standardised and predictive models of care. Private hospital networks and public health programmes are only beginning this transition, but it will be crucial if India is to extend its leadership in eye care beyond surgical volumes to long-term disease management.
Eye care is also among the fastest-growing single-specialty segments in Indian healthcare, alongside oncology. Historically, this growth has been driven by surgical volumes, which account for an estimated 80% to 85% of revenues for most eye hospitals.
“The growth of eye care in India is driven by demographic, epidemiological, and institutional shifts,” says Jain. “India’s population is aging, with more people living long enough to develop age-related conditions such as cataracts, glaucoma, and macular degeneration. Chronic systemic diseases like diabetes, where India has one of the highest global burdens, are also driving a rise in complications such as diabetic retinopathy, which require regular specialist care. Additionally, lifestyle changes are fuelling an increase in myopia as screen use rises. The way forward lies in better awareness, understanding early symptoms, and seeking regular eye check-ups.”
Workforce Shortages
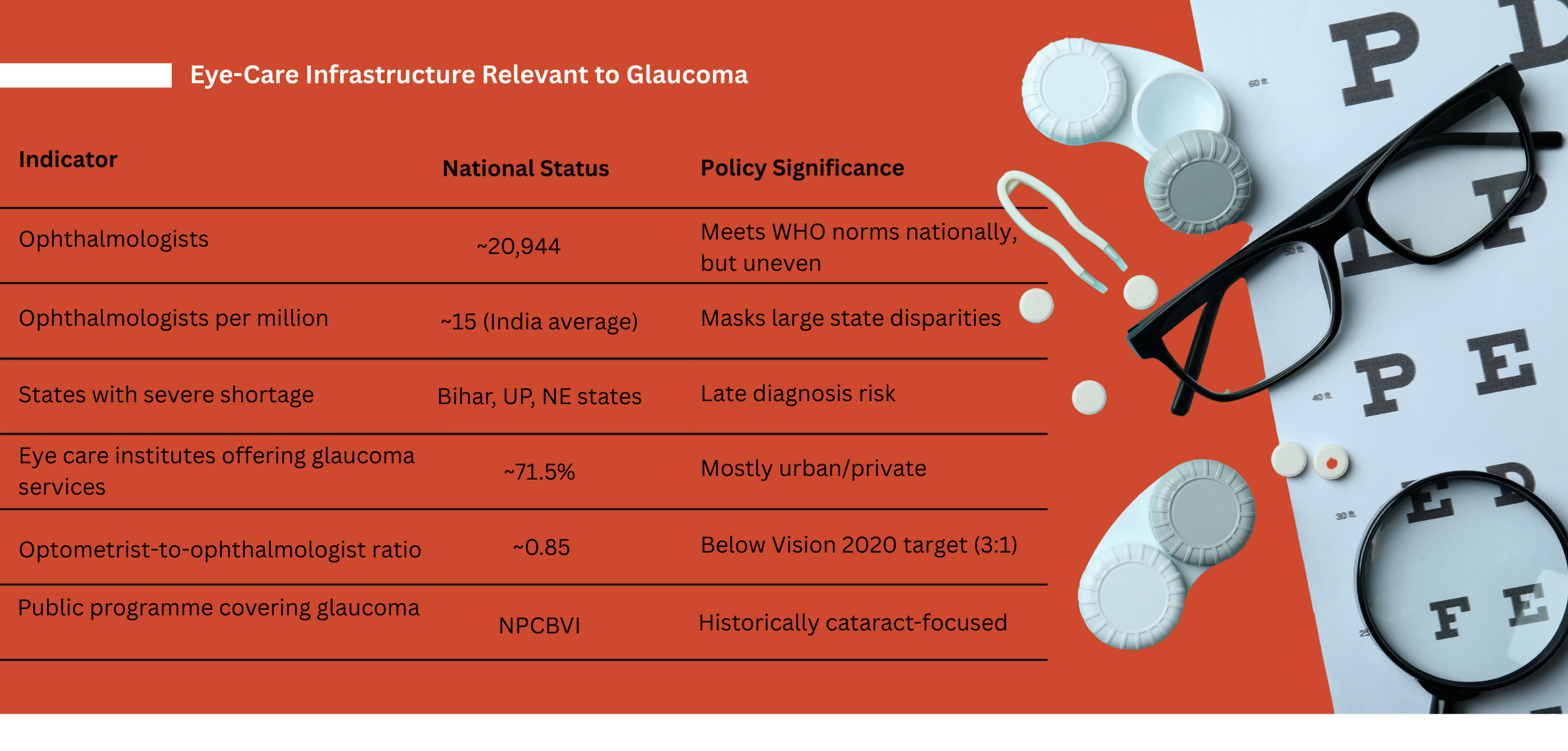
Delivering both high-volume surgery and long-term disease management depends heavily on skilled manpower. A recent AIIMS Delhi survey notes that India has, on average, one ophthalmologist for every 65,000 people. While significant progress has been made, gaps persist in workforce and infrastructure, particularly in rural and underserved areas.
India currently has 20,944 ophthalmologists and 17,849 optometrists working at secondary and tertiary levels, resulting in an optometrist-to-ophthalmologist ratio of 0.85, well below the Vision 2020 target of three paramedics per ophthalmologist.
Dr. Jain believes the solution lies in hub-and-spoke models, public-private partnerships, and better use of AI-enabled diagnostics in tier-2 and tier-3 regions. At ASG, rather than building hospitals from scratch, the group acquires small, established facilities and strengthens them with advanced technology, training, and continuous skill development. “The real asset is not the building, but the local doctor and medical team,resources that are otherwise extremely difficult to recruit,” he says. The group has also launched dedicated training programmes to address specialisation gaps.
Shifting to Provider-Initiated Care
“As a referral centre, we see the heartbreaking reality of ‘late presenters’,patients who arrive when their vision is already reduced to a narrow tunnel or is nearly gone,” says Dr. Mahavir Kandharwar, specialist in glaucoma and cataract management at the National Institute of Ophthalmology, Pune. “While affordability and follow-up are major hurdles, the single biggest gap remains early detection.”
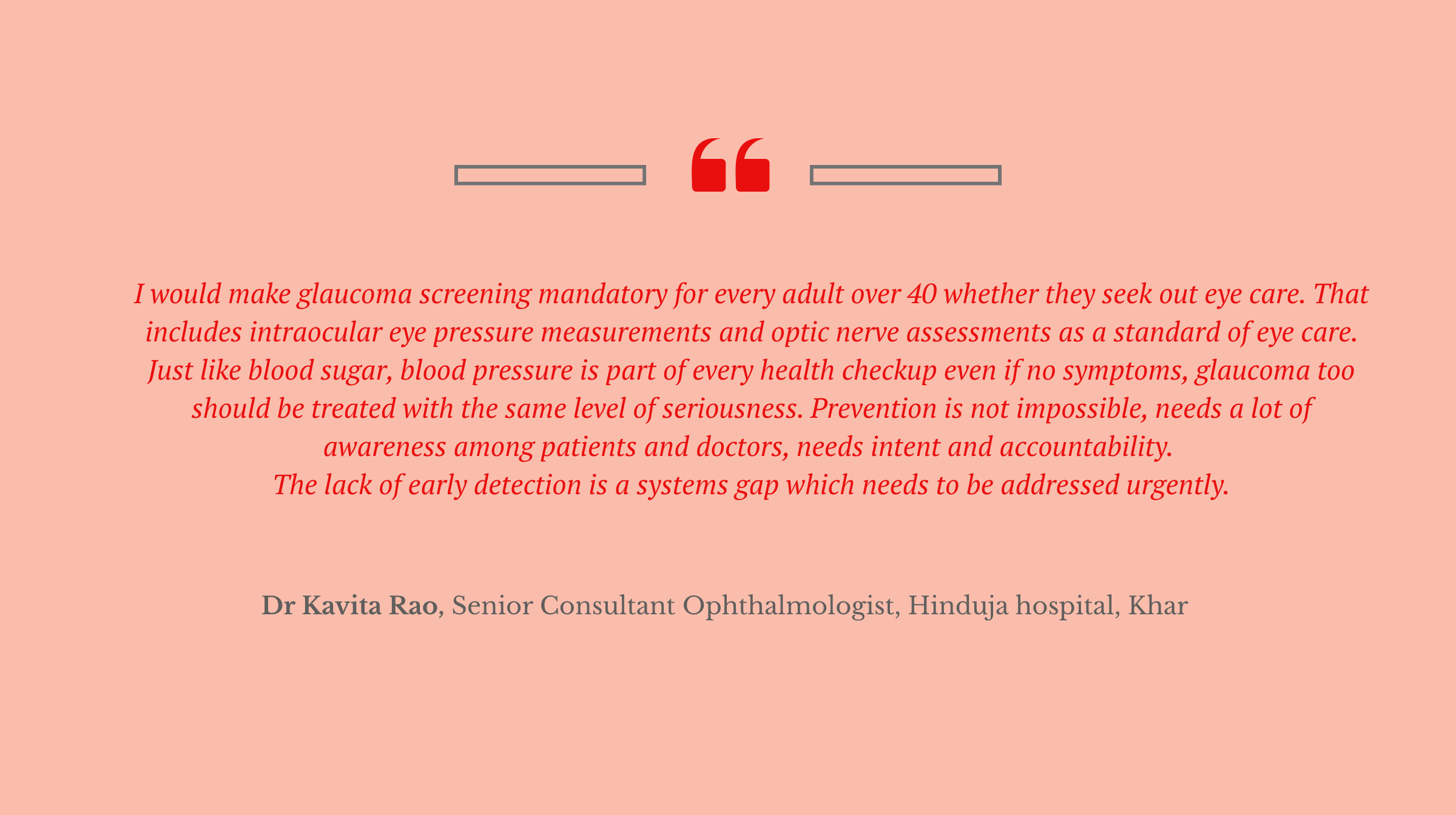
Currently, the system relies heavily on patients initiating care. “But glaucoma is asymptomatic until its end stages, so people don’t know they need help,” Kandharwar explains. “To prevent avoidable blindness, we must shift from patient-initiated to provider-initiated care.”
He advocates mandatory optic nerve evaluations for everyone over 40 seeking even basic eye care, such as reading glasses. “By integrating glaucoma screening into routine eye exams and primary healthcare, we can catch the disease at the referral stage rather than the rescue stage.”
With 11.2 to 12 million Indians affected and only 10% diagnosed, glaucoma remains the leading cause of irreversible blindness in the country. “Urban centres may have advanced technology, but rural India faces a severe shortage of specialists and diagnostic equipment, leaving referral chains broken,” Kandharwar says. “The first step is clear: timely screening and early detection are the only ways to prevent vision loss from glaucoma.”
Got a story that Healthcare Executive should dig into? Shoot it over to arunima.rajan@hosmac.com—no PR fluff, just solid leads.