Machines Can Never Replace Doctors
By Arunima Rajan
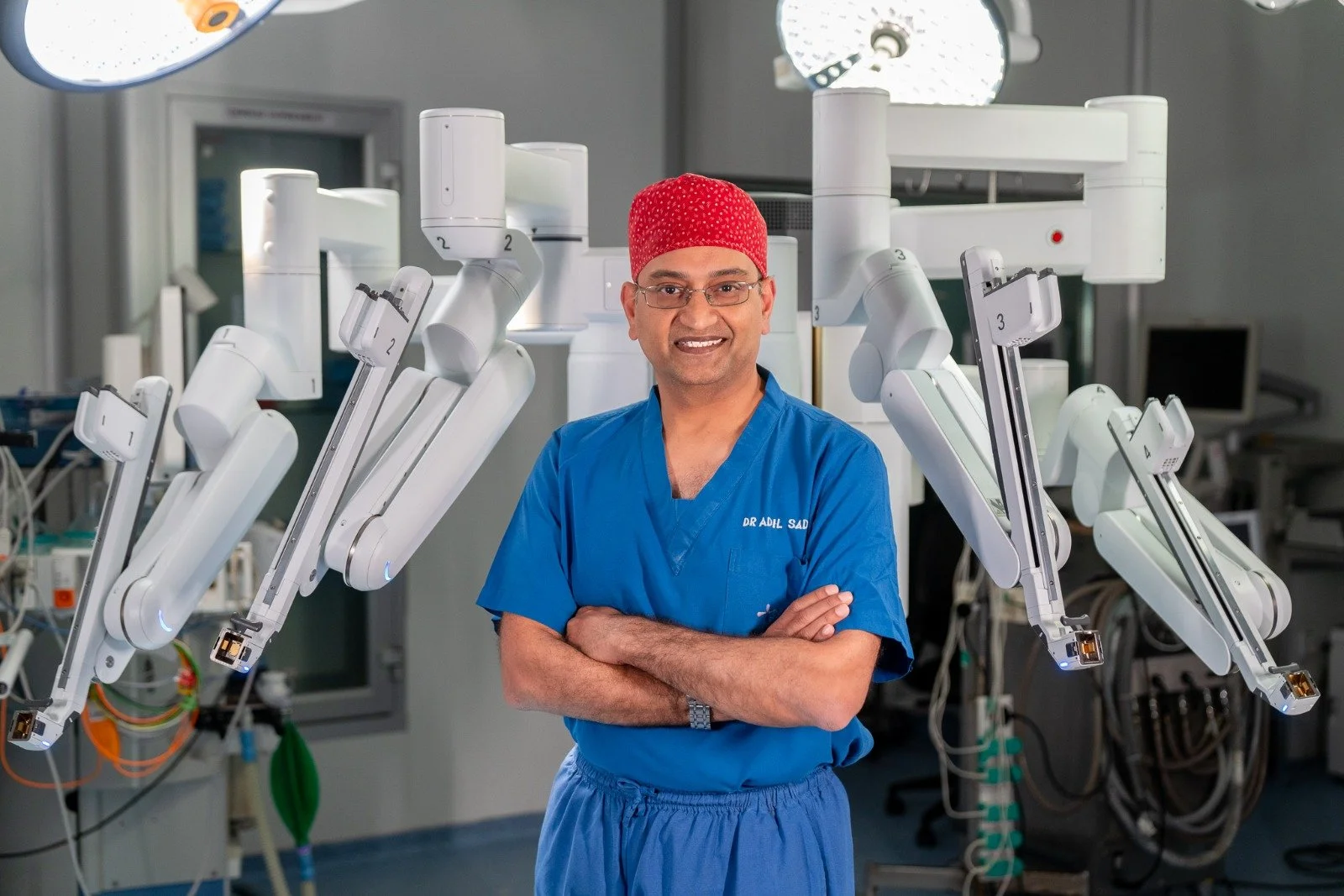
Dr Adil Sadiq
In an interview with Arunima Rajan, Dr Adil Sadiq, head of cardio-thoracic and vascular surgery at Sakra World Hospital, Bengaluru, talks about the future of AI in cardiac care.
When you tell patients that AI supported their diagnosis or monitoring, how do they respond? Do you see AI building confidence in care, or does it raise fears of “machines replacing doctors”?
Fortunately, most of the patients I see are from the educated class or are into tech, so they are quite happy that AI is being used as a medium to analyse reports. After I’ve told them that AI is supporting the diagnosis, they often ask whether I’ve also had a look at it, and the answer is always yes.
I think people are getting more and more familiar with AI, and they realise that these machines can never replace doctors, thankfully so far. But there is a certain subset of people from the lower socio-economic class who don’t understand the real impact and meaning of AI, and there’s always the apprehension that AI will or can replace doctors. There was one patient who told me that he did not want to have robotic heart surgery, and when I asked him why, he said, “Doctor, I would prefer you to do the surgery rather than a robot.”
So he had this misconception that an AI-based robot would be doing the surgery while I’d be sipping some tea or coffee.
With AI now reading ECGs and echoes at scale, do you worry that trainees and younger cardiologists may lose opportunities to sharpen their diagnostic instincts? How do you balance efficiency with skill-building?
No, I think with AI now reading ECGs, it just makes all the younger trainees much better, much more perfect in their diagnoses. AI is only a backup. Whenever we do an echo and look at what’s going on, it’s always good to put it in the AI scale to see whether we’ve missed anything or not.
So I think that’s a very important thing. We use a form of generative AI when we test the success of a bypass in heart surgery. After a bypass, we use this particular thing in an algorithm to tell how well the bypass is flowing, what the resistance is, what the quality of the anastomosis is, and it gives a rough idea of what the long-term prognosis of this bypass is.
Cardiology is shifting from hospital-centric to home-based monitoring. Do you see AI-linked wearables and remote monitoring systems changing how you follow up with heart failure or post-angioplasty patients?
I think, you know, home-based monitoring is amazing. I’ve been a big proponent of it, and I think AI wearables and remote monitoring systems will get a lot of other people under the purview of healthcare professionals.
Remember, all these send inputs, send problems and send red flags to a main data centre, which then initiates the appropriate treatment or the appropriate response. So, especially in the high-risk group of patients with heart failure or those post-heart transplant, we’ve also been using AI-based devices for our patients so that, when they go home, we track them and we get real-time data on what’s going on with them. Another group of patients for whom this is really helpful is those with continuous glucose monitoring.
For some people who have uncontrolled sugars post-op, all of which get stored in an AI-based model and get transmitted to the responsible doctor. So we have better outcomes for patients in terms of greater safety, better sugar control, better control of heart rate, prevention of abnormal heart rhythms and appropriate treatment if any of these happen.
Got a story that Healthcare Executive should dig into? Shoot it over to arunima.rajan@hosmac.com—no PR fluff, just solid leads.