Indoor Environmental Quality Check in Hospitals
By Krutikaa Sharma
Why is IEQ a vital component whilst designing hospitals?
Why IAQ check is important, particularly in hospitals?
Generally, in buildings, HVAC systems have the role to provide adequate physical comfort conditions and perceived air quality to users through fresh and conditioned air supply, heat removal and pollutant dilutions. In hospitals, the services of HVAC system extend beyond this and should also serve to prevent cross-infection risks, harmful emissions and pathogen spreading. Thus, in a hospital, the HVAC system does far more than keep occupants comfortable. It also serves a critical function in patient’s health, well-being & creates a healing environment.
Figure 1: Factors affecting IEQ of a space – Room design – Equipment-Occupants
Maintaining an environmental quality standard in hospitals is a challenge as there are several factors influencing the internal spaces. These could be related to design or equipment or occupants or all of them together.
Complex composition of departments (planning-wise & HVAC system-wise) in hospitals – Boon or Bane?
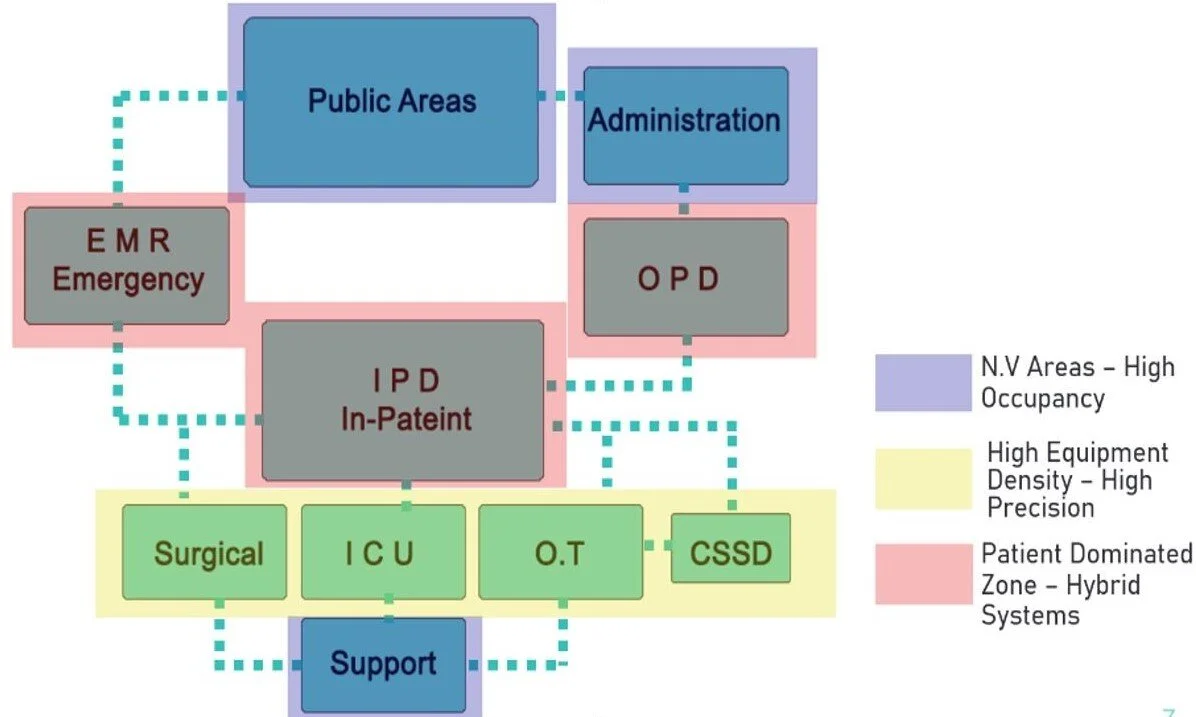
Hospitals have various departments with different functions. Along with this, the HVAC design criteria for healthcare facilities vary as much as the medical services provided. The various departments which are inter-connected would require different air distribution systems according to the varied medical services they provide. This could be managed with several configurations in the HVAC system within the hospital.
Figure 2: Composition of Departments in a hospital
The complex hospital environment requires special attention to ensure a healthy indoor air quality (IAQ) to protect patients and healthcare workers against hospital-acquired infections and occupational diseases.
Ventilation requirements are on the basis of the standards of air quality for hospitals. The standards give the values for the temperature, relative humidity, air change rates, types of filters, the pressure relationship to adjacent areas and the cases where recirculation of air is allowed. All these requirements are classified according to the purpose of the premises to meet the requirements of patients, staff and to resist the contaminant.
The standards describe general design criteria which are specified according to the various zones and their application – outpatient spaces, inpatient areas, surgical rooms, radiology, operation rooms etc. The standards give the values for the temperature, relative humidity, air change rates, types of filters, the pressure relationship to adjacent areas and the cases where recirculation of air is allowed. All these requirements are classified according to the purpose of the premises to meet the requirements of patients, staff and to resist the contaminant.
Table 1: ASHRAE Standard 170 – Design parameters
Critical areas like operating rooms where the environmental conditions need to be controlled in a more specific band for long periods, makes the design of HVAC system too critical. Indoor environmental quality (IEQ) in hospital operating rooms (ORs) constitutes a major challenge for the proper design and operation of an energy efficient hospital.
Furthermore, recommended values for the design parameters of operating room air conditioning (physiological and hygienic requirements) are given in the hospital spaces.
Figure 3: Containment zones in Critical areas e.g.: Operation Rooms
Role of efficient air filters in improving the air quality.
Air filters are known as effective devices to resist particle transmissions and trap particles in AHU systems. Preventing particles from entering the critical area is achieved with one or more stages of filtration. Minimum filter efficiencies are specified in Table 6-4 of ASHRAE Standard 170-2013. Minimum efficiency reporting values (MERV) are based on the method of testing described in ANSI/ASHRAE Standard 52.2: Method of Testing General Ventilation Air-Cleaning Devices for Removal Efficiency by Particle Size. The mechanisms by which particles are removed by fibrous filters are direct impaction, sieving (straining), interception and diffusion.
How do Filters works?
Direct impaction occurs when particles in the airstream are unable to stay with the airstream as air flows around fibers and separate from it, impacting the fiber. Because inertia increases with particle size, inertial impaction favors larger particles and is aided by higher flow velocities.
Sieving is the common intuitive mechanism of particle removal. Particles larger than the gap between fibers are trapped.
Interception occurs when a particle in the airstream collides with the fiber and is collected. That is, thanks to the inertia of the particles, they continue to move towards the fiber even as the airstream bends around it.
Diffusion occurs as a result of the rapid and random motion of small particles due to their internal thermal energies, also known as Brownian motion. As these small particles flow with the airstream, their rapid random motion can bring them in contact with the fiber and they are collected.
How and Why is Space Pressurization important?
It has been proven that overpressure of the room is reduced by mechanical means extracting an air flow lower than the driven one. This parameter favors protection of the room against cross-contamination since it induces circulation of air from clean zone to less clean corridors and adjoining rooms inside the surgical block. Over pressure in the room prevents potentially contagious bioparticles entering, complementing the filters’ work. A positive pressure of at least 2.5 Pa is the recommended minimum pressurization value that needs to be maintained at all times with respect to all adjoining spaces. Thus, an air movement from the protected area, operation room, towards the outside is achieved.
For example, for an immune-compromised/ wound intensive / burns units requires humidifiers to comply with and shall be provided with individual humidity control.
Airborne infection isolation rooms shall have a Permanently installed device and/or mechanism to constantly monitor the differential pressure between the rooms. All air shall be exhausted directly to the outdoors.
For Hazardous Room – or lab activities where the air flow needs to be cut-off, providing an air lock with + pressurization zone in the middle might help. This parameter favors protection of the room against cross-contamination since it induces circulation of air from the clean zones to less clean corridors and adjoining rooms inside the surgical block.
The purpose of positive pressurization is to define a flow pattern and to perform a particle migration barrier. A specific pressure differential at a closed door between rooms with two different air cleanliness can typically prevent airborne cross-contamination from the less clean room into the cleaner room, because even if the door frame has some minor air gaps (cracks), these openings are small and the velocities of air leakage through these cracks are high enough to prevent backflows. When the door is opened, however, the pressure differential changes quickly and the barrier’s functionality becomes questionable. In addition to the minimum required pressure differential, treatment at door-in-operation condition to prevent backflow needs to be considered.
Importance of infection control in Operation theatres
Infection Control is of Utmost importance in Operation Rooms where invasive procedures for long duration take place. Several factors affect the environment in ORs, such as
Surgical field factors – Thermal plume,
Room factors – Cleanliness
HVAC factors – ACH and Direction of Airflow
Patient factor – Susceptibility
A study conducted by Airepure to evaluate the performance of three types of ventilation systems for operating rooms with respect to air flow velocities and the Colony forming unit count (CFU) on and around the OT table. These were temperature-controlled airflow (TcAF), Laminar airflow (LAF) and turbulent mixed airflow (TMA). The different airflows of the three ventilation systems, were modelled using computational fluid dynamic (CFD) models, shown in Fig 4.
The air is introduced in the OR through a high-efficiency particulate air (HEPA) filter to dilute the contamination to a lower level. The primary difference between the three systems is the location and type of the air diffuser or panels used for the supply air. In TMA the air enters through a panel along the top of a wall in the OR and exits close to the floor in the corners of the opposite wall. Whereas, in Laminar airflow the air enters the room from a 2.75 X 2.75 m2 box above the operating table, creating an ultra-clean zone below the box, and exits through the ceiling just outside the box. In temperature-controlled airflow, the cooled and filtered inlet air is introduced from eight half-spherically shaped air diffusers mounted in a circle, creating an ultra-clean zone that expands from the centre of the room.
Airborne bacteria were measured at three locations: close to the wound, at the instrument table and in the periphery of the room. The CFU count was used as a measure of viable airborne bacterial loads.
Figure 5: Measurements taken at intervals of 0.9 m away from the operating table.
Figure 6: Clinical Evidence of Laminar Airflow.
The observations were, dramatic reduction in the airborne particle contamination, both at the operating theatre table level, and throughout the theatre. This Assessment was conducted using a calibrated particle counter.
Other aspects that can influence IEQ in hospitals are –
Finishing materials
Door Motion - the volume exchanged between two spaces due to door motion can affect the indoor air in relation to air fluxes, affect health status of individuals & increase sensory discomfort.
Anaesthetic gases leaks
Occupants – Visitors and Patients
Take Away
Therefore, even after bringing fresh air into the hospital spaces, filtering it efficiently, dehumidifying it according to the various requirements to getting it to the desired temperature, distributing this clean air according to the space pressurization is important. IEQ is an important component to the design of any building, but it’s vital whilst designing hospitals.