Nationalizing Allied Medical Curricula
By Dr. Sweta Jalan
Standardizing allied medical curricula is the key to bridging skills gap of healthcare workers, explains Dr. Sweta Jalan
Healthcare in the 21st century is about team work. The care chain involves tons of paramedical staff, without whom doctors and nurses will be quite possibly handicapped. It is the radiology technicians who operate X-Ray machines; the radiologist’s interpretation, and subsequently the treatment plan, is directly dependent on the accuracy of the image. A phlebotomist punctures the wrong vein while drawing blood and the consequences can be fatal. If a surgical technologist passes the wrong scalpel to the surgeon, the surgery will not go smooth. A large chunk of palliative care is provided by counselors, physiotherapists, exercise physiologist and occupational therapist. A primary care center in India has one doctor; the rest are non-clinicians. Their role is critical and requires appropriate specialty training.
In view of the shortage of doctors and changing health demographics, the availability of qualified human resources has emerged as a significant challenge. “There is an urgent need for the government to plug policy gaps and ensure the availability of the right human resources for quality care at primary, secondary and tertiary levels,” concludes a 2012 report released by the Public Health Foundation of India (PHFI) titled From Paramedics to Allied Health Sciences: Landscaping the journey and way forward.
Much has been said and written about the shortage of medical and nursing colleges, overshadowing the importance allied medical institutions. The existing ones lack a standard allied medical curriculum and training mechanism. According to data from National Initiative for Allied Health Sciences- Technical Support Unit, more than 955 institutes offer allied health courses in India without any standardization. And, more than 138 allied health courses are available, ranging from diplomas, graduate and postgraduate diplomas, postgraduate degree or doctorate level. But without an accreditation, how valid are these?
Non-existent Regulatory Body
Seema Jadhav
Lack of standard curricula is a direct result of lack of a regulatory body. Medical Council of India sets standard and protocols for clinicians. Similarly, Indian Nursing Council regulates nursing practices and Dental Council of India does the same for dentists. However, there is no such body that prevents unqualified allied medical staff from practicing. This has resulted in low quality care and patient safety issues in most cases. “There should be adequate number of institutes to educate and train students in allied medical professional. These institutes need to be regulated by government bodies, creating pool of employment opportunities for both skilled and non-technical professions,” says Seema Jadhav, Associate Vice President - Quality Assurance, Metropolis Healthcare Ltd.
The 2011 PHFI report was a reality check for the Indian Government. It highlighted that “better utilization of the whole range of the skills of para-professionals or AHPs is the key to health-sector reforms in India.” In lieu with the policy recommendations, the National Initiative for Allied Health Sciences was undertaken; an initiative by the Ministry of Health & Family Welfare to standardize the allied health professional education and practice in India. “The key purpose is to standardize and assure quality driven allied health services to the population by establishing the professional standards for practice, standardizing curriculum, setting standards for institutions offering such courses and for practitioners in allied health system within India.” NIAHS is also actively lobbying for establishment of Allied Health Council of India and National Board of Allied Health Sciences.
Government Initiatives
In March 2011, the Ministry of Health and Family Welfare nominated the Public Health Foundation of India (PHFI) to develop a framework to improve allied health training, education and regulation in the country.
In December 2012, PHFI released ‘From Paramedics to Allied Health Professionals’ marking the allied health training landscape including situational analysis, methodology of teaching, inputs and regulatory mechanisms for the allied health disciplines and recommending the strategic framework for the establishment of National Institute of Allied Health Sciences (NIAHS) and Regional Institute of Allied Health Sciences (RIAHS).
In December 2012, Government of India proposed to set up one National Institute of Paramedical Sciences (NIPS) at Delhi and eight Regional Institutes of Paramedical Sciences (RIPS) at Nagpur (Maharashtra), Bhopal (Madhya Pradesh), Bhubaneswar (Odisha), Chandigarh (UT), Coimbatore (Tamil Nadu), Hyderabad (Andhra Pradesh), Lucknow (Uttar Pradesh) and one location in Bihar at a total cost of INR 804.43 crore to be shared in the ratio of 85:15 between Central and the State Governments under the centrally sponsored scheme namely “Establishment of NIPS, RIPS and Supporting the State Government. Medical College for conducting paramedical courses through one time grant”
In March 2015, the Government of India made operational a Centrally Sponsored Scheme for establishment of one National Institute of Allied Health Sciences (NIAHS), eight Regional Institute of Allied Health Sciences (RIAHS) and supporting State Government Medical Colleges for conducting allied health courses to augment the supply of skilled health workforce.
Earlier this year, the Ministry of Health and Family Welfare established a NIAHS Technical Support Unit (NIAHS-TSU) to support the Ministry’s technical arm in the allied health space. The TSU has a mandate to strengthen implementation, provide policy recommendations in various thematic areas related to regulation, standardization, human resources, along with the development of standards for institutions and curricula for the allied health professions. On the basis of the mandate, the allied health section and the TSU has initiated the task of standardizing the curricula for selected allied health professional courses in phases. Curricula taskforce constituted in this regard for each professional group design and submit the curricula to the National Curricula Review Committee (NCRC) which has been constituted under the aegis of Ministry of Health and Family Welfare to support the National Initiative for Allied Health Sciences (NIAHS).
Standardization and Development of allied health system though establishment of an interim body – National Board of Allied Health Sciences on the lines of National Board of Examination is proposed and under consideration.
With this view in mind, the Ministry of Health and Family Welfare has commissioned a Centrally Sponsored Scheme for the establishment of one National and five Regional Institutes of Allied Health Sciences and to support State Government Medical Colleges for conducting allied health science courses. The first phase of the initiative undertook a massive review of the allied health landscape in the country and proposed the development of the allied health system through the establishment of an interim body called ‘National Board for Allied Health Sciences’. Currently under consideration, this process will eventually ensure the quality and standardization of the allied healthcare education and professions in the country.
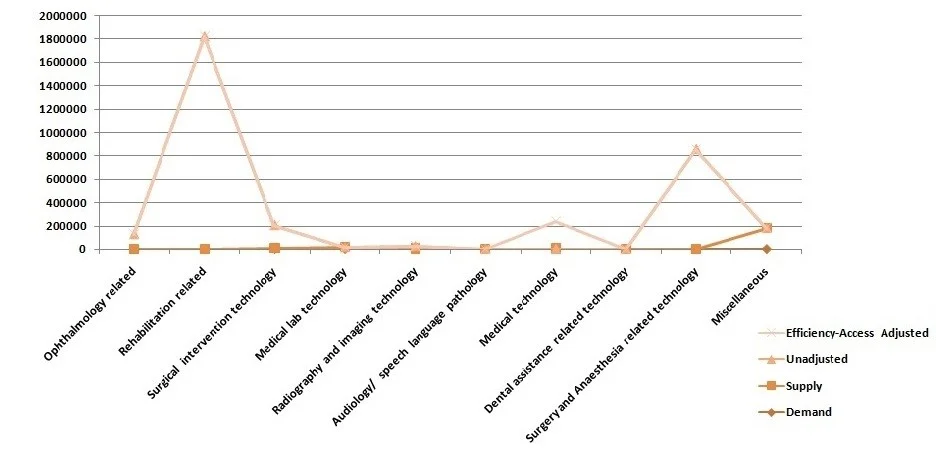
Source: From Paramedics to Allied Health Sciences: Landscaping the journey and way forward by PHFI, 2011
Data from NIAHS-TSU, Ministry of Health and Family Welfare, Government of India
Global practices in regulating allied medical profession
Australia
The Health Professions Council of Australia is the national apex body for major health professions other than medical practitioners and nurses. In Australia AHPs are regulated at the state/territory level by legislation specific to each profession. Such legislation provides for the establishment of professional boards, which oversee registration of AHPs; practice scope and standards; receipt, investigation, and action of complaints; disciplinary action and censure. Most states have undertaken recent reviews of health professional legislation – including many of the allied health professions.
USA
The allied health profession in USA is regulated by the Office of Consumer Affairs and Business Regulation (OCABR), which is under the United States Department of Labour. The organization has a dedicated Board of Registration in Allied Health profession. The Board of Registration in Allied Health evaluates the qualifications of applicants for licensure and grants licenses to those who qualify. It establishes rules and regulations to ensure the integrity and competence of licensees. The Board is the link between the consumer and the allied health professional and, as such, promotes the public health, welfare and safety.
Uganda
In Uganda, there is separate statute covering all AHP’s The Ugandan Allied Health Professionals Statute 1996 provides for the regulation, supervision, and control of AHPs, and creates an AHP Council to register and license AHPs.
Singapore
The regulation of the allied health professional in Singapore is under the allied health professional bill 2010. This bill was proposed in the Singapore parliament in 2010 and was enacted in January 2011. It intends to regulate all the allied health practitioners in the country. Initially there were 3 allied health professionals, namely: occupational therapists, physiotherapists and speech therapists which were covered under the act. The professions such as clinical psychologists, diagnostic radiographers, audiologists, podiatrists, prosthetists and dieticians will be introduced under the prerogative of the bill subsequently.
Source:
NIAHS 2015, available at http://www.niahs.org/data/Appendix
Clarke D sRaAM. consultancy report on the regulation of allied health professions (AHPS) in ECSA region. Commonwealth regional health community secretariat for east, central and southern Africa, April, 2003. Report No.
Australia THPCo. The Allied Health Professional Workforce in Australia: Challenges and Opportunities
Varying Training Standards
Since a regulatory body is absent, the allied medical curricula and training methods grossly vary from institution to institution. Quality of education also suffers due to the faults in faculty, infrastructure and content. At the faculty level, at present, there is no defined criteria for the qualification and classification of the faculty. For AHPs, India largely relies on training-the-trainer model. Institution offering allied health education in India range from government-affiliated universities, distance-learning universities to public and corporate hospitals, medical equipment manufacturing firms and even pharmaceutical companies Hence courses are often customized to meet the institution’s human resource needs. In terms of content and training methods, NIAHS reports that there marked difference between the private and public sectors. Also, for the same skills set, a range of courses exist at various institutions; for example, medical laboratory technology (MLT) can choose a one-year course, a certificate, a two-year diploma, and a three-year degree programme. With the establishment of HSSC, there is a some amount of harmonization in courses. P.D. Hinduja Hospital offers six one-year postgraduate allied medical courses, namely CSSD Technician, MRD Technician, OT Technician, Advanced Medical lab technician, Dialysis Technician, Radiology Technician and Physicians Office Assistant. Joy Chakraborty, COO, P.D. Hinduja Hospital, takes pride in saying that all are developed in conjunction with the HSSC guidelines.
With rapidly evolving medical technology and emerging micro-specialties, continuous professional developments have become even more imperative but far too few are available. A good example to emulate would be that of Metropolis, which employs a dedicated learning and development team, to enhance overall growth and career of an employee. Metropolis is one of them. “Training & Development is an on-going process here. We have a dedicated learning and development training team. There are defined set of policies and procedures for training, CMEs, competence assessment for all the laboratory staff. A training plan is developed for each role, based on which the performance of an employee is monitored,” shares Seema.
Let’s take the example of US anesthesiologist assistants. US has ten accredited anesthesiologist assistant training programs. Approximately 97 percent of currently practicing anesthesiologist assistants hold a Master’s degree. Upon completion of the educational program, graduates must sit for a credentialing exam that is co-validated by the National Board of Medical Examiners and National Commission for Certification of Anesthesiologist Assistants. All anesthesiologist assistant programs are credentialed by the Commission on Accreditation of Allied Health Educational Programs (CAAHEP).
Confusing Designations and Restricting Prospects
AHPs have varied definitions and job roles in different countries. Australia uses the term speech pathologist, whereas the United States uses a ‘speech language pathologist’ and the same is called a speech and language therapist in United Kingdom. “In India, the lack of standardization in nomenclature, job roles, career pathways etc. also fails to attract students to pursue higher education and there is mounting evidence of student opting out of health sector,” states NIAHS. Even if they do pursue a higher degree, return on investment is very poor, resulting in a redundant career pathway. Furthermore, they have limited employment options in the Government institutions. Very little data is available on the role of specific allied health professional towards the healthcare delivery and treatment outcomes. Better appreciation for their qualification by sensitizing all stakeholder of healthcare will encourage more students to opt for this profession and add to dignity of labor. Seema advises, “Government should introduce new schemes and sponsor scholarship for students who intend to pursue their career in respective areas of interest. Efforts should be made to explore ways to bring new people into healthcare careers and to increase the capacity to train new health professionals.”
The Rule of In-house training
Mr. Joy
Without an accredited degree, hospitals are skeptical to trust their skills and most undergo in-house training. This is another reason for students to not pursue a degree in AHP. It could seem pointless. Traditionally, healthcare has always been viewed as being doctor-centered; recruiting unqualified allied medical staff and training them in-house is an accepted norm. Many paramedics work as unlicensed assistive personnel, i.e. they serve the patient under the supervision of qualified healthcare professional and hold no accredited degree. “Allied medical education is not standardized in India. Hence, it is a gamble to recruit staff based solely on educational qualification. Rather than qualification, we recruit paramedical staff based on qualification and past professional experience. However, in-house training differs from hospital and hospital, setting to setting. Even the experienced recruits need some level of in-house training. The freshers are 100 percent in-house trained,” says Joy. Realizing the need for it, P.D. Hinduja started formal (certified) courses for allied medical staff.
Even diagnostic chains need a horde of paramedical staff for operating radiology equipments, drawing blood for blood test, pathological testing etc. Seema says that though they recruit based on qualification, they are not confident of their skills unless they are trained in-house. “The laboratory has pre-determined qualification required for each and every position that has been set in place. For example, in order to be a technician the candidate’s should have completed a course or a diploma in DMLT. It is ensured that every resume is screened and scrutinized even before the candidates are called for an interview for the respective profile. Orientation is an introduction to the organization, the job and the community. Our staffs are very much dependent on in-house training, because these are skill-based activities. The training is directly related to skills, knowledge and strategies necessary to do a particular job. A comprehensive in-house training program is planned for each department once a month to update them with the latest developments and know-how.”
Quantity with Quality
Allied medical education is currently rudimentary and untamed. As the Government aims to train 150 million AHPs by 2022, without establishing an autonomous central accreditation body that minds that standards of allied medical education, their contribution cannot reach its true potential.